- NYC UES Office
- 970 Park Avenue, Suite GFN,
New York, NY 10028
- Carnegie hill Office
- 1175 park avenue,
new york, ny 10128
What is Bone Grafting?
Over a period of time, the jawbone associated with missing teeth “atrophies” or is reabsorbed. This often leaves a condition in which there is poor quality and quantity of bone suitable for the placement for dental implants. 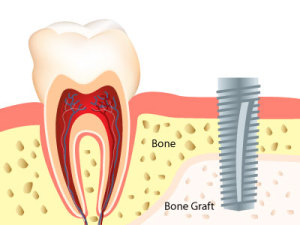
Today, we have the ability to grow bone where needed. Dental bone grafting rebuilds the jawbone and makes it suitable for dental implants. This not only gives us the opportunity to place implants of proper length and width, it also gives us a chance to restore functionality and aesthetic appearance.
What are the Types of Bone Grafting Procedures for Dental Implants?
There are various types of bone graft procedures, described as follows:
1) Sinus Lift Procedure– This procedure involves elevating the sinus membrane in the back area of the upper jaw and placing the bone graft on the sinus floor. Dental implants can then be successfully mounted in the newly stable bone.
2) Ridge Augmentation- Ridge augmentation involves rebuilding the bone height at the area where the dental implants will be placed. The width or thickness of the ridge may also be increased when necessary. A ridge augmentation is accomplished by placing bone graft material in the tooth socket. It is often done immediately after the tooth is removed, to avoid the need for a second procedure later
3) Socket Bone Preservation– In socket bone grafting, a bone graft is placed in this extraction socket to maintain the bone level necessary for future implant placement. While not always necessary, socket bone grafting allows for more predictable bone formation in anticipation for dental implant procedures.
How Do I Know If I Need Bone Grafting?
After a comprehensive oral exam to determine the necessity of a dental bone graft, Ruben Cohen, DDS performs several diagnostic tests using Cone Beam Computer Tomography (CBCT) or Computed Tomography (CT) scans to determine the precise quantity and quality of bone available. These tests provide an image of the affected area, and indicate the exact amount of damage that has occurred due to the defect.
What are the Different Types of Bone Grafts?
Autogenous Bone Grafts: Autogenous bone grafts, also known as autografts, are made from your own bone, taken from somewhere else in the body. The bone is typically harvested from the chin, jaw, lower leg bone, hip, or the skull. Autogenous bone grafts are advantageous in that the graft material is live bone, meaning it contains living cellular elements that enhance bone growth. However, one downside to the autograft is that it requires a second procedure to harvest bone from elsewhere in the body. Depending on your condition, a second procedure may not be in your best interest.
Allogenic Bone: Allogenic bone, or allograft, is dead bone harvested from a cadaver, then processed using a freeze-dry method to extract the water via a vacuum. Unlike autogenous bone, allogenic bone cannot produce new bone on it’s own. Rather, it serves as a framework or scaffold over which bone from the surrounding bony walls can grow to fill the defect or void.
Xenogenic Bone: Xenogenic bone is derived from non-living bone of another species, usually a cow. The bone is processed at very high temperatures to avoid the potential for immune rejection and contamination. Like allogenic grafts, xenogenic grafts serve as a framework for bone from the surrounding area to grow and fill the void.
Both allogenic and xenogenic bone grafting are advantageous in that they do not require a second procedure to harvest your own bone, as with autografts. However, because these options lack autograft’s bone-forming properties, bone regeneration may take longer than with autografts, with a less predictable outcome.
What are Bone Graft Substitutes?
As a substitute to using real bone, many synthetic materials are available as a safe and proven alternative, including:
Demineralized Bone Matrix (DBM)/Demineralized Freeze-Dried Bone Allograft (DFDBA): This product is processed allograft bone, containing collagen, proteins, and growth factors that are extracted from the allograft bone. It is available in the form of powder, putty, chips, or as a gel that can be injected through a syringe.
Graft Composites: Graft composites consist of other bone graft materials and growth factors to achieve the benefits of a variety of substances. Some combinations may include: collagen/ceramic composite, which closely resembles the composition of natural bone, DBM combined with bone marrow cells, which aid in the growth of new bone, or a collagen/ceramic/autograft composite.
Bone Morphogenetic Proteins: Bone morphogenetic proteins (BMPs) are proteins naturally produced in the body that promote and regulate bone formation and healing.
Synthetic materials also have the advantage of not requiring a second procedure to harvest bone, reducing risk and pain. Each bone grafting option has its own risks and benefits. Dr. Cohen will determine which type of bone graft material is right for you.
What are Other Common Causes for Bone Grafting?
The following are the most common causes for jawbone deterioration and loss that may require a bone grafting procedure:
Tooth Extractions: When an adult tooth is removed and not replaced, jawbone deterioration may occur. Natural teeth are embedded in the jawbone, and stimulate the jawbone through activities such as chewing and biting. When teeth are missing, the alveolar bone, or the portion of the jawbone that anchors the teeth in the mouth, no longer receives the necessary stimulation, and begins to break down, or resorb. The body no longer uses or “needs” the jawbone, so it deteriorates and goes away.
Periodontal Disease: Periodontal diseases are ongoing infections of the gums that gradually destroy the support of your natural teeth. Periodontitis is affected by bacteria that adhere to the tooth’s surface, along with an overly aggressive immune response to these bacteria. If gingivitis progresses into periodontitis, the supporting gum tissue and bone that holds teeth in place deteriorates. The progressive loss of this bone, the alveolar, can lead to loosening and subsequent loss of teeth.
Dentures/Bridgework: Unanchored dentures are placed on top of the gum line, and therefore do not provide any direct stimulation to the underlying alveolar bone. Over time, the lack of stimulation causes the bone to resorb and deteriorate. Because this type of denture relies on the bone to hold them in place, people often experience loosening of their dentures and problems eating and speaking. Eventually, bone loss may become so severe that dentures cannot be held in place even with strong adhesives, and a new set may be required.
Trauma: When a tooth is knocked out or broken to the extent that no biting surface is left below the gum line, bone stimulation stops, which results in jaw bone loss. Some common forms of tooth and jaw trauma include: teeth knocked out from injury or accident, jaw fractures, or teeth with a history of trauma that may die and lead to bone loss years after the initial trauma. A bone grafting procedure would be necessary to reverse the effects of bone deterioration, restoring function and promoting new bone growth in traumatized areas.
Misalignment: Misalignment issues can create a situation in the mouth where some teeth no longer have an opposing tooth structure. The unopposed tooth can over-erupt, causing deterioration of the underlying bone. Issues such as TMJ, normal wear-and-tear, and lack of treatment can also create abnormal physical forces that interfere with the teeth’s ability to grind and chew properly. Over time, bone deterioration can occur where bone is losing stimulation.
Osteomyelitis: Osteomyelitis is a type of bacterial infection in the bone and bone marrow of the jaw. The infection leads to inflammation, which can cause a reduction of blood supply to the bone. Treatment for osteomyelitis generally requires antibiotics and removal of the affected bone. A bone graft procedure may then be required to restore bone function and growth lost during removal.
Tumors: Benign facial tumors, though generally non-threateningly, may grow large and require removal of a portion of the jaw. Malignant mouth tumors almost always spread into the jaw, requiring removal of a section of the jaw. In both cases, reconstructive bone grafting is usually required to help restore function to the jaw. Grafting in patients with malignant tumors may be more challenging because treatment of the cancerous tumor generally requires removal of surrounding soft tissue as well.
Developmental Deformities: Some conditions or syndromes known as birth defects are characterized by missing portions of the teeth, facial bones, jaw or skull. Dr. Cohen may be able to perform a bone graft procedure to restore bone function and growth where it may be absent.
Sinus Deficiencies: When molars are removed from the upper jaw, air pressure from the air cavity in the maxilla (maxillary sinus), causes resorption of the bone that formerly helped the teeth in place. As a result, the sinuses become enlarged, a condition called hyperneumatized sinus. This condition usually develops over several years, and may result in insufficient bone from the placement of dental implants. Dr. Cohen can perform a procedure called a “sinus lift” that can treat enlarged sinuses.